Oral cancer, it’s more than smoke & mirrors
Learn about the importance of early oral cancer detection, risk factors, screenings, and managing treatment side effects though the personal story of a dental hygienist who’s been ther
I woke up in a hurry like most mornings to get ready for work, kissed my husband goodbye, and headed out the door. About two hours later, I got an SOS call from him. “Babe, I woke up with a huge knot on the side of my neck. It hurts to swallow. I’m scared.”
That was the phone call that changed another aspect of my life. You see, my husband was critically injured in the line of duty several years ago, which resulted in a kidney-pancreas organ transplant. He ended up having to have the transplant kidney removed 7 years later. Before that incident, he had been a smokeless tobacco user for about 20 years. As a current dialysis patient along with past immunosuppression medication use from the transplant, his physician assumed he had a systemic infection but knew lymphoma was a possibility. As a dental hygienist, I thought maybe he might have a nasty abscess. So, while his physician started antibiotics, I had him come into the office for radiographs and an oral cancer screening. No abnormalities were seen that day. Not even a week later, he was diagnosed with Squamous Cell Carcinoma of the Left tonsil confirmed via biopsy. The cause was immunosuppression, HPV 16+, and prior smokeless tobacco use. As a hygienist, I felt like I failed. However, instead of focusing on the negative, I threw myself into learning all I could to help my husband through this diagnosis. I had to be a better advocate for not only him but for my patients, to make sure I was doing my due diligence in educating them on the risks, symptoms, and treatments of oral cancer. In addition, I had to make both the extra and intraoral cancer screenings a priority at every appointment with my patients as well as educate them about the human papillomavirus.
Risk factors and symptoms
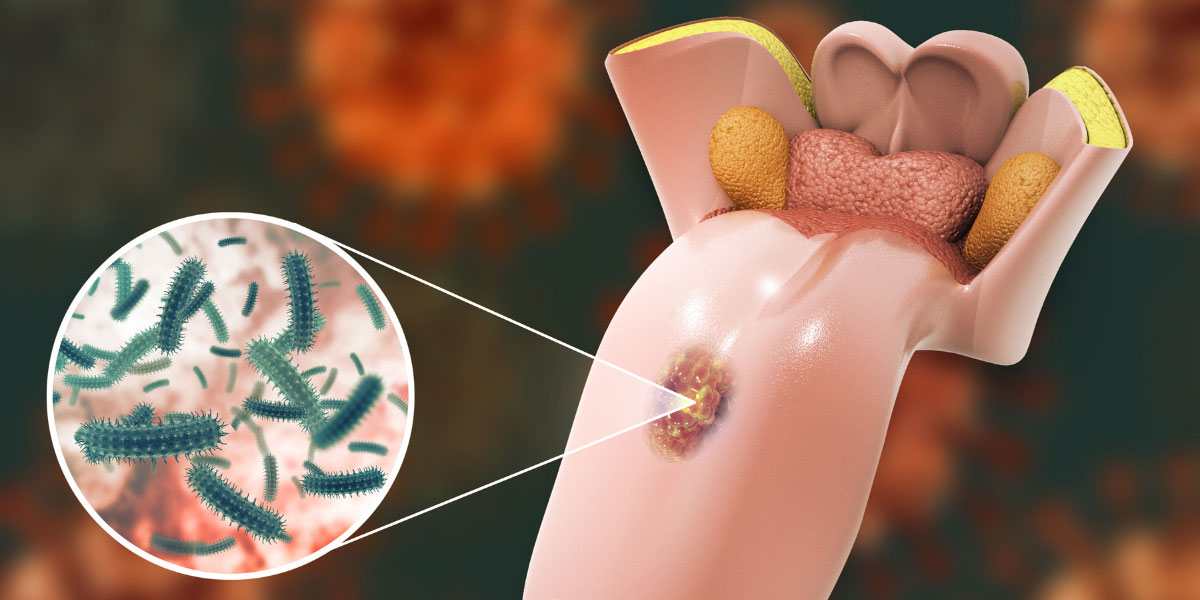
As an organ transplant recipient, you are made abundantly aware of the statement, “It is not a matter of if you get cancer, but when”. Taking immunosuppressive medications is known to increase your chances of getting cancer. Most often it is a skin cancer, so imagine our surprise to learn he had oral cancer. As a hygienist, I have been taught the risk factors and pathology but I still had much to learn. Such as, did you know that one does not have to have any known risk factors to have oral cancer? Cancer is non-biased, but when one thinks of oral cancer they often relate it to tobacco. It turns out, tobacco and heavy alcohol use, immunosuppression, family history, and the human papillomavirus (HPV) are all risk factors. The high-risk strains HPV16 and HPV18 are the main strains which contribute to oral cancer and it is more common in men vs women over the age of 40 [1].
When oral cancer is caught early, there are successful outcomes. Hence, it’s essential to know the symptoms could include ulcers and persistent sores that do not heal within two weeks, an enlarged lymph node of the cervical chain of the neck, pain, unexplained weight loss, fatigue, and difficulty swallowing or speaking. As oral cancer progresses symptoms could also include bleeding, pain, or numbness in the mouth and loose teeth [2]. The rule of thumb is if you see or feel something suspicious and it does not heal or go away in two weeks let your medical provider know. In my husband’s case, we let his physician know right away due to the size of the enlarged lymph node and pain.
Oral Cancer screening
At every comprehensive exam, it is required to conduct an oral cancer screening, but what about conducting a screening at your follow-up or future dental cleaning appointments? Your dental hygienist and dentist should be providing a thorough extraoral and intraoral examination at least twice a year. During the screening, one should expect both an extraoral and intraoral examination. During the intraoral exam, all areas of the tongue, tissue, salivary glands, tonsils, and back of the throat are viewed. We are looking for a white or red patch of the gums, tongue, tonsil, or lining of the mouth, a hard-painless lump in the cheek, near the retromolar pads or the front teeth, irregular color or growth of tissue, or an open sore that does not go away [2]. The extraoral exam should include palpation of your jaw, throat, neck, and back of your head to evaluate any enlarged lymph nodes or cysts.
Did you know you could screen yourself for oral cancer at home? As a woman, we are told to self-examine ourselves for breast cancer. All individuals are told to look out for abnormal moles, and skin tags for skin cancer. So why are we not looking in our mouths for signs, or abnormalities that could be cancer? The best way to evaluate yourself at home is to look in the mirror for any changes to the skin and palpate the throat, the sides of your neck and the back of your head, including behind the ears. Then take a small flashlight and look in your mouth at both sides of the tongue, and the back of the throat. Keep in mind there are abnormal structures in the mouth that are harmless, such as tori and geographic tongue.
You have oral cancer, what now?
Talk to your medical and dental provider. Your radiation oncologist should inquire about your last dental exam, which is necessary before starting treatment should one’s oral cancer treatment plan include chemotherapy and radiation. Do you have any infections, decay, or gum disease? All crucial questions are due to the damaging effects radiation will have on the oral cavity. The truth is radiation burns! It damages the tissue to eradicate the cancer leaving painful sores, mucositis, and severe xerostomia which may lead to the patient having a feeding tube placed due to the pain experienced when eating. In worst-case scenarios, symptoms can result in future gross caries and osteonecrosis. Your dental provider can prepare you by providing any necessary restorative treatment, extractions, prescription fluoride toothpaste, and magic mouthwash. In addition, your dental hygienist can go over your home care plan which may include the fabrication of fluoride trays, and recommending xerostomia products in the form of gums, rinses, sprays, and gels to alleviate your symptoms.
Every cancer experience is different and may require less or more support. My husband is an oral cancer survivor with residual effects from radiation exposure including short episodes of paralysis to the left side of his tongue. There were plenty of times when he wanted to end treatment due to the pain. Fluoride trays had been made but the types of gel attempted for use were irritating to his tissues and due to his severe xerostomia, he could not take the pain. Therefore, other products were given to attempt to alleviate those symptoms. I say this because it will take some trial and error to get your overall care plan right but following the steps below were taken for his case. His care plan included brushing more frequently, rinsing his mouth every 4 to 6 hours with a non-hydrogen or non alcohol mouth rinse, using magic mouth rinse when necessary, and moisturizing lips with Aquaphor or Vaseline. It is important to note there is a waiting period before applying a chap-stick before radiation therapy[3]. Avoiding spicy foods, citrus, tobacco, and alcohol is also necessary to avoid additional discomfort with radiation therapy.
Catching oral cancer early has a high cure rate. Knowing what to look for and knowing how to care for your symptoms is imperative to one’s success in completing treatment. If diagnosed with oral cancer there will be help along the way. You got this!